Introduction
For a long time, persons on nearly any insurance plan have been surprised with unexpected bills after routine preventive colorectal cancer screening procedures. They might go to sleep for a regular screening colonoscopy and wake up with a bill for a diagnostic or therapeutic colonoscopy due to findings or additional procedures that took place during the screening.
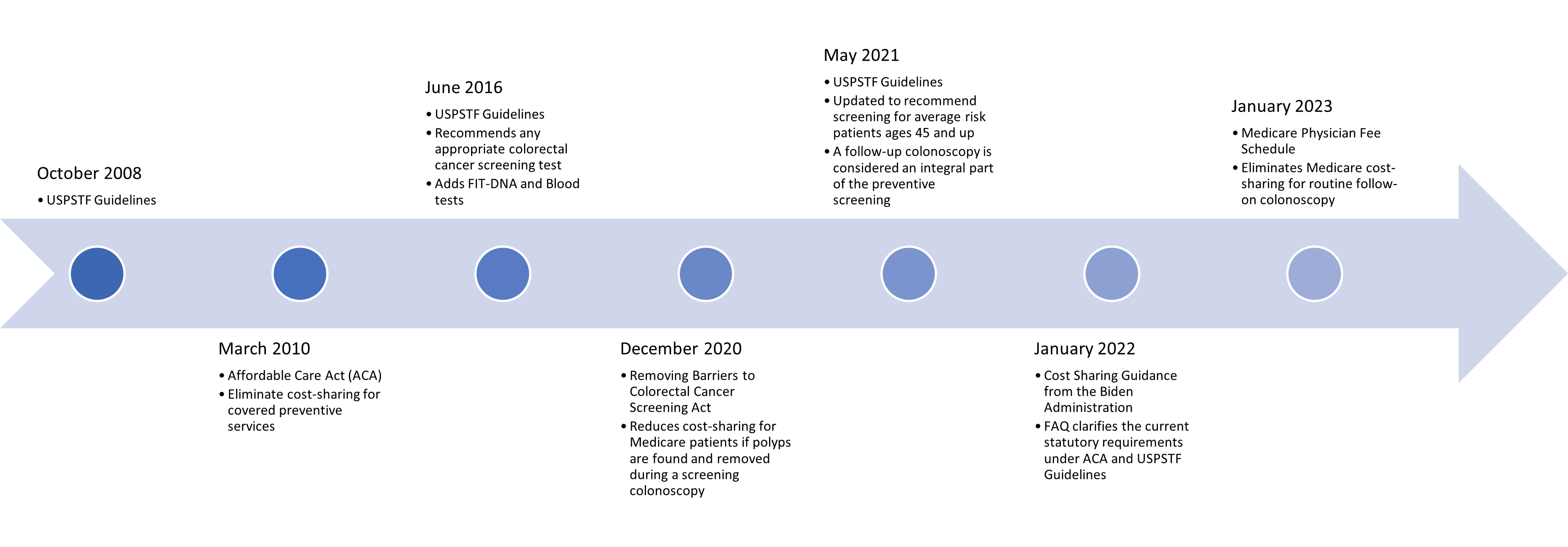
March 2010
In 2010, the Affordable Care Act (ACA) was signed into law. One of the goals of the ACA was to eliminate cost-sharing for covered preventive services recommended by the United States Preventive Services Task Force (USPSTF). As far as Colorectal Cancer (CRC) Screening is concerned, the latest guidance was published in 2008.
Because the ACA references the USPSTF, changes in recommendations published by the USPSTF are applicable by law and must be implemented within one year of the publication.
June 2016
In 2016, the CRC Screening recommendations were updated by the USPSTF, acknowledging the importance of any appropriate CRC screening test rather than focusing on the efficacy of specific tests. In addition, FIT-DNA (Cologuard®) and DNA Blood tests were added to the list of screening modalities.
December 2020
The ACA does not apply to traditional Medicare or Medicaid plans, nor does it apply to plans created before the ACA was enacted, known as “grandfathered” plans. To better align Medicare with the USPSTF Guidelines, in 2020, the Removing Barriers to Colorectal Cancer Screening Act was signed into law, reducing the cost-sharing Medicare beneficiaries if polyps are found and removed during a screening colonoscopy. This was implemented with a phased approach, reducing the cost-sharing by 5% every two years until 2030, when that cost-sharing is eliminated entirely.
May 2021
In 2021, the USPSTF Guidelines were updated again, this time to add an additional age group, 45-49, to the recommendation. In addition, the USPSTF further clarified that a “follow-up colonoscopy” is now considered an “integral part of the preventative screening, without which the screening would not be complete.” This is an important clarification that will have a profound impact on the way screening is performed and measured in the future. Because these recommendations were published in May 2021, ACA health plans must comply with these changes by May 2022; in effect, health plan or policy years starting after May 2022 must include these changes.
January 2022
Again, the ACA references the USPSTF. By this time, significant changes have been made to the USPSTF Guidelines, and additional clarifications are needed for health plans and issuers to maintain compliance with the ACA. To this end, the Biden Administration released a cost-sharing guidance document in the form of Frequently Asked Questions (FAQs) that clarifies the statutory requirements under the ACA and USPSTF Guidelines. In particular, the document identified that a follow-up colonoscopy and all related services, such as polyp removal, pathology, and associated office visits, is considered a step of the screening process and should result in no cost-sharing.
January 2023
Again, the ACA does not apply to traditional Medicare, Medicaid, or grandfathered health plans. However, in January 2023, Medicare published their Physician Fee Schedule (PFS), which takes the USPSTF Guidelines into effect on Medicare plans. As a result, there is no cost-sharing for any of the USPSTF recognized screening modalities or “follow-on” colonoscopies. The only exception is if there are additional services required during a follow-on colonoscopy, such as tissue removal, those services will continue to be billed in accordance with the Removing Barriers to Colorectal Cancer Screening Act (2020).
Conclusion
As a result of these changes, after May 2023, all commercial ACA plans, also known as “metallic” or marketplace plans, will cover all appropriate colorectal cancer screening modalities at 100% for average and high-risk patients when performed at appropriate intervals, including any necessary follow-on colonoscopies and related procedures. Beginning January 2023, all traditional Medicare plans will cover all appropriate colorectal cancer screening modalities and follow-on colonoscopies at 100%, with exception to additional services, which are currently paid at 85% and will be 100% beginning January 2030. North Dakota Medicaid Expansion pays the same as an ACA plan, and North Dakota traditional Medicaid should be treated like a grandfathered plan.
Resources
Billing Modifiers: Reducing or Eliminating the Cost Barrier for Colorectal Cancer Screening
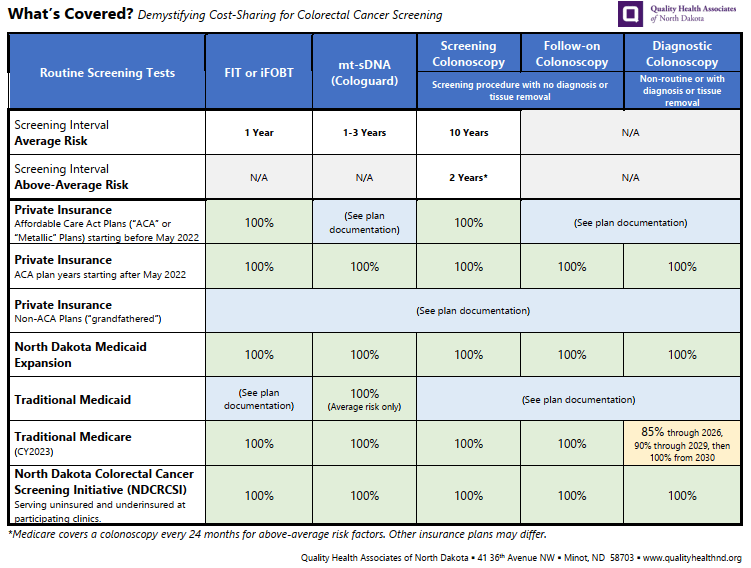
What’s Covered? Demystifying Cost-Sharing for Colorectal Cancer Screening (Updated January 2024)
Updated Cost-Sharing Guidance for Medicare Beneficiaries
Colorectal Cancer Screening: New Cost-Sharing Guidance
News
No post found!